Takayasu arteritis
Definition
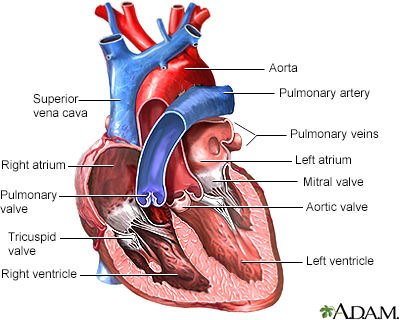
Takayasu arteritis is an inflammation of large arteries such as the aorta and its major branches. The aorta is the artery that carries blood from the heart to the rest of the body.
Alternative Names
Pulseless disease, Large-vessel vasculitis
Causes
The cause of Takayasu arteritis is not known. The disease occurs mainly in children and women between the ages of 20 to 40. It is more common in people of East Asian, Indian or Mexican descent. However, it is now being seen more often in other parts of the world. Several genes that increase the chance of having this problem were recently found.
Takayasu arteritis appears to be an autoimmune condition. This means the body's immune system mistakenly attacks healthy tissue in the blood vessel wall. The condition may also involve other organ systems.
This condition has many features that are similar to giant cell arteritis or temporal arteritis in older people.
Symptoms
Symptoms may include:
- Arm weakness or pain with use
- Chest pain
- Dizziness
- Fatigue
- Fever
- Lightheadedness
- Muscle or joint pain
- Skin rash
- Night sweats
- Vision changes
- Weight loss
- Decreased radial pulses (at the wrist)
- Difference in blood pressure between the two arms
- High blood pressure (hypertension)
There may also be signs of inflammation (pericarditis or pleuritis).
Exams and Tests
Possible tests include:
- Angiogram, including coronary angiography
- Complete blood count (CBC)
- C-reactive protein (CRP)
- Electrocardiogram (ECG)
- Erythrocyte sedimentation rate (ESR)
- Magnetic resonance angiography (MRA)
- Magnetic resonance imaging (MRI)
- Computed tomography angiography (CTA)
- Positron emission tomography (PET)
- Ultrasound
- X-ray of the chest
Treatment
Treatment of Takayasu arteritis is difficult. However, people who have the right treatment can improve. It is important to identify the condition early. The disease tends to be chronic, requiring long-term use of anti-inflammatory medicines.
MEDICINES
Most people are first treated with high doses of corticosteroids such as prednisone. As the disease is controlled the dose of prednisone is decreased.
In almost all cases, immunosuppressive drugs are added to reduce the need for long-term use of prednisone and yet maintain control of the disease.
Conventional immunosuppressive agents such as methotrexate, azathioprine, mycophenolate, cyclophosphamide, or leflunomide are often added.
Biologic agents may also be effective. These include TNF inhibitors such as infliximab, etanercept, and tocilizumab.
SURGERY
Surgery or angioplasty may be used to open up narrowed arteries to supply blood or open up the constriction.
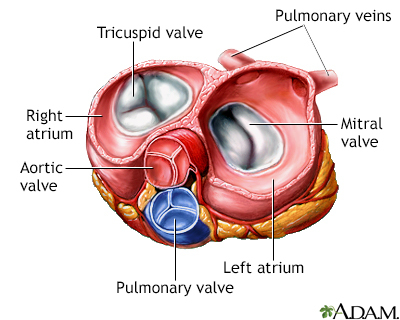
Aortic valve replacement may be needed in some cases.
Outlook (Prognosis)
This disease can be fatal without treatment. However, a combined treatment approach using medicines and surgery has reduced death rates. Adults have a better chance of survival than children.
Possible Complications
Complications may include:
- Blood clot
- Heart attack
- Heart failure
- Pericarditis
- Aortic valve insufficiency
- Pleuritis
- Stroke
- Gastrointestinal bleeding or pain from blockage of bowel blood vessels
When to Contact a Medical Professional
Call your health care provider if you have symptoms of this condition. Immediate care is needed if you have:
- Weak pulse
- Chest pain
- Breathing difficulty
Gallery

References
Alomari I, Patel PM. Takayasu arteritis. In: Ferri FF, ed. Ferri's Clinical Advisor 2022. Philadelphia, PA: Elsevier; 2022:1460-1460.
Ehlert BA, Abularrage CJ. Takayasu disease. In: Sidawy AN, Perler BA, eds. Rutherford's Vascular Surgery and Endovascular Therapy. 9th ed. Philadelphia, PA: Elsevier; 2019:chap 139.
Hellman DB. Giant cell arteritis, polymyalgia rheumatica, and takayasu's arteritis. In: Firestein GS, Budd RC, Gabriel SE, Koretzky GA, McInnes IB, O'Dell JR, eds. Firestein & Kelley's Textbook of Rheumatology. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 93.
